|
It's Holiday gift giving time! But do you really need another sweater or pair of socks from your aunt? Or what about that hard-to-buy for relative? NO! Who needs more stuff!? What you really need is to help midwifery in Missouri stay legal and protected by a donation to the MMA Lobbyist Fund. We'd like to raise 3,000 to finish paying him for this year and start the fund for next year. If we can't make it, then the MMA will not be able to hire him next year and that means risking that bad bills will get passed restricting or eliminating the practice of midwifery in Missouri. Midwives do not have the deep pockets that those in the medical establishment have. Having a lobbyist for the MMA helped tremendously in the last two legislative sessions. Consider donating as a gift for someone or share the link for family members to donate as a gift to you. Every bit helps and won't cause consumer clutter! And everyone will feel great that they helped keep midwifery legal and accessible in Missouri. Thank you!
Donate to the Missouri Midwives Association Lobbyist Fund
0 Comments
Columbia Area Midwives is pleased to invite you to free screening of the latest home birth documentary movie: “Why Not Home? The Surprising Choices of Doctors and Nurses.”
This is a family friendly event and snacks will be provided. Thank you to Erica Kroll of Nona Birth Education and Counseling for hosting this event. __________________________________________ Date: November 17th, 2016 Time: 7:00 pm to 9:00pm Location: Nona Birth Education and Counseling 1204 Rogers St. Columbia, MO 65201 Cost: Free! After the film, we will have time for Q & A and discussion. ________________________________________________ Why Not Home? tells the stories of doctors, nurses, and midwives who have attended hundreds of hospital births, yet chose to have their children at home. How did these women with inside knowledge of hospital based birth evaluate the evidence and make their decisions? Through the experiences of these women, both at home and in the hospital, we gain unique insights into risk, safety, and the experience of childbirth in America. Here is a link to the film’s website: http://www.whynothome.com/ _______________________________________________ Please share this invitation widely, RSVP on the Why Not Home Facebook event page, and bring a friend! We look forward to seeing you! 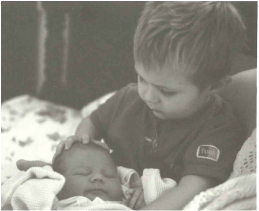 Ian holds his sister Isolde the evening she was born at home Ian holds his sister Isolde the evening she was born at home Granted, I am biased, but in no particular order, here are five things I think are particularly wonderful about home births and midwifery care. Supporting women in labor with whatever kind of support they desire If a woman desires complete silence with no moving around while she is having a contraction, or if she asks me to kneel on her lower back while she is on all fours because she wants that much counter pressure during a contraction—she gets it. I love adapting and supporting a laboring woman in whatever way she discovers she needs, whether it is hands on, hands off, praying, singing, silence, or verbal encouragement. Witnessing women being forces of nature That’s how I describe it. The raw power of labor and birth are simply magnificent. I am in awe of every woman dealing with contraction after contraction in her own unique rhythm as she builds in power to push her baby into the world. Even if things don’t go as expected and we have to transport to hospital, these women have given 150% by this time and handle the change in plans with such strength and stamina. Women are simply amazing. Birthing positions and places: One size doesn’t fit all! Standing, sitting on a birth stool, squatting, laying down, side-lying, hands and knees, on the stairs, in the tub, in the bathroom, in the living room, in the bedroom, outside! These are positions and places women have given birth. What will work best for you? I don’t know, let’s find out! Instead of being maneuvered into the typical “sit-on-your-sacrum-feet-in-stirrups” position that is mainly for the doctor’s benefit; at a home birth, a woman is encouraged try out many different positions for second stage. Some positions really do work better than others for bringing a baby down and out so when the woman’s work of birth is supported, rather than a doctor’s convenience, births go more smoothly for mother and baby. Welcoming babies with care and respect As the newest member of the human species, making the transition from watery environment to air-breather-land dweller in a matter of mere minutes, a new baby deserves some respect! For a normally adapting baby, the typical routine procedures like suctioning out the airway, immediate cutting of the cord, and separation from the mother quickly after the birth are unnecessary. I love that babies get the loving care that keeps them with their mothers in home births. Family togetherness I have witnessed so many wonderful moments of older siblings meeting their newest family member for the first time--the gentle fascination for tiny hands, soft skin, and fuzzy hair! When this happens in the loving familiarity of the home and not the strange environment of the hospital, I believe it helps children adapt better. Because midwives give postpartum care in the home in the days to come, the older children continue to witness and sometimes “help” with these visits. Newborn babies are fascinating and I love answering question children have –most commonly about the newborn’s umbilical stump! There are many more things I love about midwifery care and home birth, but I will keep to five things for now. What did you love about your midwifery care and/or home birth? “What is your transport rate?” During interviews between a midwife and a potential client, this is a common question. The straightforward interpretation is: ‘in your practice, how many women do you end up taking to the hospital during labor from their planned home birth?”
This question is more complex than it would first seem and to tease apart the layers gives more insight than answering with a simple percentage. To do that in any meaningful way, you need studies that can look at large numbers. One of the more recent studies looked at planned, midwife attended home births between 2004 to 2009 and found that the overall transport rate during labor was 10.9 %. However, this number may not accurately represent a midwife with a small home birth practice. The frequency of transporting to the hospital for any individual midwife has more to do with the demographics of her practice. If a midwife has a client base of mostly women for whom the pregnancy is not the first baby, then her transport rate is likely to be very low. If a midwife has all first time mothers as clients, that will make for a high looking transport rate. Age can also be a factor: women who are in their upper 30s who are having a first baby have a higher rate of transport than women of the same age range having a consecutive baby. A midwife’s level of skill also plays a part. It would be expected that a newly launched midwife, whose goal is to practice safely, would transport with a bit more frequency than someone who has had years of experience. A seasoned midwife simply has more skills at her disposal with a more nuanced eye to evaluate what situation can be worked with at home and when it becomes necessary to go in. The legality of the practice of midwifery in one’s particular state will also affect the transport rate. States in which the practice of midwifery is illegal or are hostile to midwife-attended home births create an environment in which midwives and their clients are fearful about transporting. They may wait too long to go in resulting in a lowered number of transports but ones of a more serious nature. The safest home birth and midwifery practice environments are places where midwifery is legal, where midwives can consult and transport freely without fear of legal repercussion for simply seeking timely help. Built into this question, I feel, is an underlying assumption that transporting to the hospital is a bad thing. Of course, if someone is planning a home birth, we all want that to be successful with no need to go to the hospital. However, there are times during the course of the labor when it becomes clear that a baby is simply not going to be born at home. Most likely it is due to a stalled labor that needs some kind of assistance after everything has been tried at home to make that happen. So, if that is the case, after a laboring woman and her team of supporters and care providers have tried everything and had a discussion of options, then going to the hospital is a prudent choice, a necessary choice, and even though can be a disappointing turn of events, it isn’t a “bad thing.” There are a couple more points the question of transports bring. What if, during your interview with a midwife, she relates that she never or rarely ever transports? It’s possible that she is a very experienced midwife with a practice of women in their mid-twenties, none of whom is having a first baby. Or perhaps she is simply telling you what she believes you want to hear? It would be worth asking a few more questions to figure this out. A woman seeking midwifery care should be looking for a reasonable and thoughtful approach to complicated labors that need to transport, not something sounds like an implied guarantee that births will always happen at home. If birth teaches us anything, it is that none of us are in the driver’s seat for this most common of miracles. Other than the skills and knowledge that a midwife appropriately uses for an individually unfolding labor and birth, she ultimately has no control over how a labor will go. Yes, there are some women who, statistically, have a higher chance of needing to transport, but no midwife carries a crystal ball in her birth bag, and the hopefulness of “defying the odds,” for an otherwise healthy, low-risk woman, deserves a real chance (called a ‘trial of labor’ in technical terms). Midwives are sometimes surprised, in hindsight, of who ended up successfully birthing at home and who ended up needing to transport. Statistics can tell some of the story but they can’t always tell your story. Even though the question of transporting can’t be answered in a meaningful way with a flat number, it still deserves to be discussed during an interview with a home birth midwife. Better questions to ask are: What are some reasons women in labor transport? Who is more likely to need to transport and why? What skills do you have to try to work with those situations so that a transport won’t be necessary? How do you know when it is time to transport? How do you handle a transport? The best we can hope for and continue to work toward is for providers of all levels of care, from home birth midwife to high–risk obstetrician, to be able to communicate and collaborate so the most appropriate level of care is easily accessible for any pregnant woman at any stage of this journey.  This week's blog post is courtesy of the Columbian Missourian's "From Readers" column. I was delighted to be invited to write a story and I tried to share some information about home birth and midwifery care interwoven with a personal story. Dawn Finney is a certified professional midwife and owner of Birthroot Midwifery in Columbia. “Why don’t you just have the baby in the hospital?” This was the question my father posed to me when I told him, 19 years ago, that I was planning to have my second baby at home. I was on the telephone nervously sharing with my parents my plans, and essentially, my hopes for this birth to be different than my first, which had been medically managed and hadn’t gone as I had imagined. Even so, I still appreciated the care I received from the certified nurse midwife who attended to me at the large university hospital in Iowa. I remember a moment, after the profundity of bringing my beautiful son into the world, in which I looked at my midwife and thought: “I need to do what she’s doing.” My path to midwifery was different than hers, though. I did attend nursing school, for a short time thinking I would pursue a master’s degree in nurse-midwifery and work in a hospital as most CNMs do. However, I was fortunate to meet a wonderfully skilled midwife who apprenticed me for four years, including a midwifery internship program in St. Petersburg, Russia. I earned my Certified Professional Midwifery credential, joining the ranks of the only type of maternal health care provider with training specific to the out-of-hospital birth environment. “But you can have your insurance pay for the birth in the hospital,” said my father. Ever practical, he voiced concern for the expense we would incur as a graduate-student family living on one income. Yet, this kind of maternity care offered quality and value that was worth paying out-of-pocket for: hour-long appointments with plenty of time to talk about my concerns and ask questions, care that respected my choices and treated me like an individual, privacy and comfort of being in my home instead of being at the mercy of policies and procedures decided by board rooms of lawyers, and postpartum care complete with breastfeeding support that came to my home when I needed it. The fee we paid our midwives was a fraction of the cost of a hospital birth for empowering care that felt priceless. In Missouri, there have been yearly efforts to license the legal practice of CPMs in the hopes that this would allow insurance reimbursement for midwifery care and planned home birth. If accomplished, it could save millions of dollars as it has in other states with licensed midwifery. “Call us when you go into labor so I know when to start worrying.” Now my mother was on the phone with me and I know that, in her own way, she was supporting my decision to birth at home. Worry. It’s a rare person who doesn’t feel some degree of this emotion when embarking on the journey to bring a baby into the world. Indeed, “what if something goes wrong” is a question that must be addressed whenever a couple comes to the complimentary interview appointment at which I discuss the option of midwifery care and home birth. If the couple does not bring this up, I do. The main risk of home birth is encountering a complication in which speedy access to a hospital is necessary. In reality, that kind of emergency is less common than our cultural fear about birth would have us believe. The most frequent reason to transport to a hospital is the opposite problem: a prolonged labor that has stalled and needs augmentation. A strong component of midwifery training is learning to recognize and manage any complications of birth and transporting to hospital when necessary. As I came to learn through my own birth experiences and my work as a midwife, a big driver of women choosing home birth is a less-than-satisfying birth experience in hospital with interventions that felt coerced or possibly unnecessary. Women having a first baby often choose home birth because they know they have a 33 percent chance of having a C-section just by giving birth in a hospital. Ultimately, I explain that no labor and birth is totally risk-free, no matter where a woman gives birth. What couples need to sort out is which set of risks do they want to choose? The good news is that for both hospital and home birth, the vast majority of births result in successful outcomes for mothers and babies. “Well, I guess that’s OK,” concluded my father. “I was born at home, too.” It turns out that a traditional midwife welcomed him and some of his siblings into the world. My daughter was born, not too long after this conversation, in the comfort of my own home under the care of skilled midwives. It has been my great honor to continue the legacy of providing midwifery care for planned home birth that was once common for all of our families. Link: Columbian Missourian "From Readers" Home birth legacy continues with local midwife I occasionally get emails from young women who are interested in becoming a midwife. It’s great that the idea of midwifery seems to be spreading in the younger generation; perhaps becoming more of a modernized household word. There are some important considerations when thinking about one’s path to midwifery. In this article, I explore some of these ideas in a general way. This is by no means an exhaustive discussion. At the end, I’ll include links to resources that may help the aspiring midwife in her research.
First, what many who inquire about midwifery may not realize is that there are two educational tracts in the US for becoming a midwife. There are some interesting historical and political reasons why this is so, but that may be a topic for the future. Direct-entry midwifery is the term that represents the more traditional style of apprenticeship training. A student spends a number of years learning under the guidance of a more experienced midwife until she is ready to practice on her own. The student is responsible for obtaining the didactic portion of her education either through a program of study set out by her senior midwife or a long-distance educational program. Clinical experience in midwifery can also be gained by attending internship programs in the US or other countries. The requirements to be a CPM continue to evolve as the credential undergoes more standardization through agencies that accredit this route of education. The student has the option of testing for the national credential of Certified Professional Midwife which is administered by the North American Registry of Midwives. In twenty-six states, the CPM is recognized as the legal credential to practice out-of-hospital midwifery. The CPM is the only midwifery credential with training specific to the out-of-hospital birth environment. There are also brick-and-mortar midwifery schools, which may also offer a long-distance learning option with periodic clinical components for which the student must travel. For a student midwife wishing to earn a CPM credential, the school must meet the guidelines set by the Midwifery Education Accreditation Council (MEAC). Graduation from such a program fully prepares a student to take the NARM exam. CPMs who earned the credential under older guidelines must complete a bridge program by 2020 that will grant compliance with MEAC. Certified Nurse Midwife is the credential earned by students who have gone through formal education in nursing and have attained a master’s degree in nurse midwifery. CNMs are licensed and legal in every state although practice regulations differ from state to state making some states more difficult for the CNM to function in the full scope of her practice. Most CNMs work in hospital-based practices although some do have home birth practices. Having described the two routes for aspiring midwives, let me say that there is no easy way to become a midwife. Education and training in midwifery takes time, commitment, and hard work--as it should. I am a firm believer in rigorous midwifery training which includes a full scope of skills appropriate to the practice of midwifery. Your heart may make it very clear which route to take, but if you are weighing your options, I’d like to offer some thoughts for consideration. While the idea of training in the traditional apprenticeship model and being a home birth midwife may sound attractive, it can be difficult to find a midwife that will take you as an apprentice or be able to provide you the clinical practice opportunities if you are going through a MEAC approved school. If you find a midwife who can take you on, the volume of her practice needs to be high enough to give you the degree of experience or numbers you need to complete your training in the time allotted. If not, you may need to travel to a clinical site elsewhere to get the numbers and experience you need. Students earning a CPM credential must consider the laws of the state in which they wish to live. There are a handful of states in which the practice of midwifery is a felony and this can make it difficult to advertise or practice openly. A state with licensure for CPMs may make it possible for midwives to bill insurance companies; thus increasing the volume and financial stability of the practice. The nursing school route is generally more accessible and straightforward as a path to midwifery. CNMs are legal in all states, although again, you will want to consider the laws of the particular state in which you wish to live as some states restrict the practice of nurse-midwifery. Opportunities will also vary across the country as some cities have hospitals with thriving CNM practices, but many do not. Being a CNM (and a master’s degree level nurse at that) will offer more flexibility and employment opportunities to be able to earn a good income. I often encourage young women who contact me about midwifery to consider nursing for their educational route for those reasons. It’s possible, but a little less common, for CNMs to have a home birth practice. The laws of a particular state and the need to pay off student loans can be determining factors in this choice. Some CNMs get their CPM credential (or vice versa) to be able to have a home birth practice. Having both credentials is certainly one way to have all bases covered when it comes to the variability of midwifery practice environments. As a CPM, I love the ability I have to practice in a way that respects and honors the physiologic process of labor and birth. I am to able to be practical and responsive to the individually unfolding needs of the labor and birth of each woman. I value a model of care that didn’t need to be approved by a boardroom of men and that isn’t at the mercy of policies and procedures that were only designed with potential litigation in mind. And yet, I imagine that were I a CNM, I would have the ability to reach many more women with the midwifery model of care in populations that could benefit from it. Working in a structured environment with support of other professionals just down the hall, some kind of scheduled work life with a dependable income, health insurance, and a retirement plan are benefits I don’t get by being a self-employed CPM. In the meantime, there are other great things you can do as you research or prepare for your educational route. You can become a doula—this is a great way to learn about labor and birth, find out what goes into being a support person for a childbearing woman, get a feel for what being on-call is like, and gain some experience on the business side of being a birth worker. In my area, Nona has an excellent doula training program. Join your state midwifery organization. Get involved with the effort your state has to make or keep midwifery legal and viable. Here in Missouri, visit: Missouri Midwives Association. Below are additional resources: North American Registry of Midwives Midwives Alliance of North America Midwifery Education Accreditation Council American College of Nurse Midwives When it comes to hospital birth in the USA, we have many wonderful technological advancements that can do a great deal of good when it comes to keeping mothers and babies healthy and safe. After a birth, hospital postpartum care makes sure mothers and babies make normal transitions in this important time, that the needed newborn tests are done, and by the time a swaddled bundle is placed in the mother’s arms as she makes her way to the car to go home, all is well.
However, this is just the beginning of life with a new baby, and the beginning of a mother’s continued healing and adjustment after the momentous act of giving birth. There may be other children at home and a partner that needs to get back to work all too soon. The new baby gets follow up appointments, of course: well-baby check ups and weigh-ins if necessary. However, mothers are not seen again until the six-week postpartum visit unless there is a problem. What if that problem was preventable with some post partum visits for the mother? What if there was someone coming to visit the mother and new baby to help with things like breastfeeding, or checking on uterine and perineal healing? What if someone came to her home to ask how she is feeling and offer remedies for postpartum blues? And what if there was someone to assist the new mother to get extra help, community support, or a referral to another care provider so a small problem can get solved before it turns into a bigger one? Our institutionally-based maternal and newborn health care system does many good things, but postpartum care is not one of them. It leaves mothers to fend for themselves in what is, in American culture, an often isolating experience. There is a solution, though. Certified Professional Midwives know that birth is really the beginning of everything. Good postpartum care is essential to the healthy continuum of a woman’s childbearing cycle. What does this look like? Midwives come to the home to comprehensively assess the mother and baby’s well-being at regular visits. Midwives help with breastfeeding as much as needed. Midwives get late-night phone calls from clients asking for help and then go to the home to help. What physician or nurse is going to do that? You can’t get better or more responsive postpartum care than with a midwife. In a medical system that undervalues this important area of health care, Birthroot Midwifery fills this gap. I am happy to let everyone know that I offer a package of postpartum care services (home visits and much more!) that can be contracted by those who are having hospital births. Please check my Postpartum Services page for more information. Mothers and babies deserve midwives! |
Midwife's musings...A midwife must possess a lady's hand, a hawk's eye, and a lion's heart. ~Aristotle Archives
December 2017
Categories |
Proudly powered by Weebly


 RSS Feed
RSS Feed